65yr old man case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
HOPI:-
A 65yr old man , farmer by occupation came with complaints of involuntary movements of bilateral upper and lower limbs lasting for about 3 to 5 minutes.
Patient was apparently asymptomatic till morning and has done his daily activities without any fail. Then his attender noted him developing sudden onset of involuntary movements of bilateral upper and lower limbs which are tonic type lasting for 3 to 5 minutes. This activity is associated with uprolling of eye balls amd frothing. Post ictal confusion lasted for about 5minutes and he has no memory of that event.
No history of tongue bite, bowel amd bladder incontinence , loss of consciousness.
No h/o alcohol intake before seizure activity
No history of shortness of breath, chest pain, fever, pedal edema, decreased urine output, blurring of vision. No history of Weakness of limbs, loss of sensations.
No h/o loss of smell, deviation of mouth, slurring of speech., difficulty in breathing and swallowing.
He became normal after the activity without any interventions or any medical help. They came to hospital after 2hrs of the event and no such similar activities are noted in between.
*Past history:-
- no similar complaints in the past.
-- not a k/c/o HTN, DM, TB, ASTHMA, CAD, CKD,EPILEPSY
-- no past surgical history
* Personal history :-
He takes a mixed diet with good appetite and regular bowel and bladder habits. He gets adequate sleep and is a chronic alcoholic since 10 years drinking approximately 100ml toddy per day and chronic smoker since 5yrs 2beedis/day .
Family history:- not significant. No similar complaints in family.
General examination:-
At the time of presentation patient was comfortably lying in his couch, conscious coherent , co operative and oriented to time ,place and person. There were no involuntary movements noted.
VITALS:-
TEMP - 98F
PULSE- 116bpm, regualr , normal in volume
BP -- 110/80mm of hg
RR -- 18 breaths per min
SPO2-- 99% at room air
GRBS -- 173mg/dl
No sings of pallor, icterus , clubbing, cyanosis, koilonoichia, lymphadenopathy,edema.
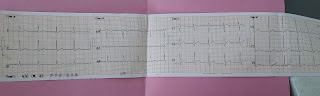
CVS:- S1, S2 heard, normal, no murmurs
RS :- BAE+ , NVBS+, no added sounds
PER ABDOMEN :- soft, scaphoid,non tender,no organomegaly, no free fluid, all hernial orifices are normal, bowel sounds are heard.
CNS:-
-HMF- intact
- CRANIAL NERVES -- all cranial nerves are normal
-MOTOR SYSTEM RT LT
Bulk -- normal normal
Tone -- UL normal normal
LL normal normal
Power UL 5/5 5/5
LL 5/5 5/5
Reflexes
Biceps + +
Triceps + +
Knee ++ ++
Ankle + +
Plantar normal normal
- SENSORY SYSTEM
Sensation, Vibration , Proprioception are intact
- CEREBELLUM :- intact., no abnormality
- GAIT :-
The patient had gross left genu valgum since his childhood. They deny any history of trauma, swelling or pain in both knees.
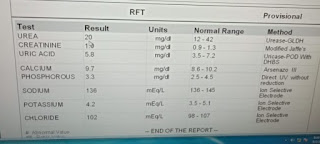
INVESTIGATIONS:-
Depending on his condition the following investigations have been done.
Day 1:-
1.HAEMOGRAM:-
Hb- 11.1gm/dl,TLC:- 9,100cells/cu.mm, RBC- 3.83million/cu.mm PLATLETS:-1.91Lakhs/cu.mm
SMear showed normocytic normochromic blood picture.
2. CUE:-
Clear, pale yellow, straw coloured urine with specific gravity 1.010., with ALBUMIM- TRACES, SUGARS - NIL, BILE SALTS-NIL, PUS CELLS- 2-4,NIL RBC.
3.RBS-- 149mg/dl
4.SERUM POTASSIUM:- 3.7mmol/litre
5.MRI BRAIN
LFT
DAY 2
OPHTHAL REFERRAL:- for changes of papilloedema. And optic neuritis because that might be a focus for seizure activity and is a finding which cannot be seen in MRI BRAIN
DAY 3:-
1.FASTING LIPID PROFILE
2.THYROID PROFILE
Under 3days of observation there was no new activity of involuntary movements and no fresh complaints from patient.
*TREATMENT GIVEN:-
1.INJ.OPTINEURON 1ampoule in 100ml NS IV BD
2.TAB.LEVIPIL 500MG BD PO
3. TAB.PANTOP 40mg OD PO
4. TAB.ULTRACET BD PO
5.TAB.MVT OD PO
Pt. Got discharged and on discharge the following medications are advised
1.TAB.LEVIPIL 250mg 4days treatment
Day 1 and 2 250mg BD
Day 3 and 4 250mg OD and stop
2.TAB. SODIUM VALPROATE 300mg OD
3.TAB PANTOP 40mg OD x 5days
4 TAB.ULTRACET BD x 5days
5.TAB MULTIVITAMIN OD x 10days








Comments
Post a Comment