Medicine case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
HOPI
Pt. Was apparently normal 10days ago , then developed gradual onset weakness , progressive in nature in B/L UPPER LIMB AND LOWER LIMB.
He also reported one episode of fever spike (low grade) subsided on medication 2days ago. Next day morning , pt. was going back to home on bike during which he had giddiness and unable to move his limbs and ride furthur. So he stopped and took rest on road during which he collapsed . Then he was seen by a bypasser who then informed his family members after which they took him to home and called an RMP to his home.
No h/o trauma , external injuries. RMP gave him few injections and tablets. Next day he came to Kamineni OPD.
Pt. Even complaints of dragging type of pains in B/L UL AND LL., since 10days. Tingling present. No ,c/o numbness and paresthesias
Pt. Initially had weakness in pressing accelerator while driving car since 10days then after 5days notices decrease in hand grip and unabke to lift weights( which he had carried before eg. Bag of vegetables, rice bag). But no history of difficulty in climbing stairs., mixing food., no h/o difficulty in getting up from squatting posture. No difficulty in combing hair. No bowel and bladder incontinence. No difficulty in buttoning and unbuttoning.
No h/o diplopia , blurred vision ., anosmia., no facial deviation, drooling of saliva. No difficulty in swallowing., speech and breathing. No h/o ataxia and difficulty in walking. No gait abnormalities.
H/o low back ache
h/o difficulty in getting up from lying in bed,in mornings after getting up from sleep. Has stiffness in body for atleast 30min. Which resolves on itself.
no h/o difficulty in holding pen/buttoning/unbuttoning
no h/o difficulty in breathing
no h/o difficulty in lifting the head off the pillow
no h/o difficulty to roll over the bed
no h/o involuntary muscles
no h/o fasciculations/muscle twitchings
h/o slippage of chappal while walking without knowledge
no h/o sensory deficit in feeling clothes
no h/o sensory deficit for hot/cold
no h/o tingling and numbness in UL & LL
no h/o band like sensation
no h/o trauma
no h/o giddiness while washing face
no h/o cotton wool sensation
no h/o urgency/hesitancy/increased frequency of urine
no h/o urinary incontinence
h/o fever/
No h/o nausea/ vomiting/diarrhea
no h/o seizures
no h/o spine disturbances
no h/o head trauma
no h/o loss of memory
no h/o abnormality in perception of smell
no h/o blurring of vision
no h/o double vision/difficulty in eye movements
no h/o abnormal sensation of face
no h/o difficulty in chewing food
no h/o difficulty in closing eyes
no h/o drooling of saliva
no h/o giddiness/swaying
no h/o difficulty in swallowing
no h/o dysphagia/dysphasia
no h/o tongue deviation
no h/o difficulty in reaching objects
no h/o tremors/tongue fasciculations
no h/o incoordination during drinking water
no h/o fever/neck stiffness
Past history:
no h/o similar complaints in past
not a known case of DM/HTN/EPILEPSY/CVA/CAD
Past Surgical:- pt.has undergone a surgery of ORIF WITH PLATING of right radius as a treatment for right radius fracture
personal history:
mixed diet with normal appetite and normal bowel/bladder movements
H/o smoking since 10yrs., 10 to 15 cigarretes/day
Not an alcoholic
no significant family history.
Pt. Is not allergic to any foods and any drugs he has consumed till now
General examination:
Moderately built ; moderately nourished
afebrile
Pallor absent
Icterus negative
No cyanosis,clubbing,lymphademopathy,Edema.
no short neck
no scars;no h/o tropic ulcers
no neurocutaneous markers
Bp 120/80 mmhg.rt. hand sitting position
Pr 80 bpm, regular, normal volume
CNS :--s1 s2 hears no murmurs
RS :-- bae + nvbs heard., no added sounds
P/a soft ,nontender
CNS:-
{DAY 1}
HMF
oriented to place/time/person
no h/o aphsia/dysarthria
no h/o dysphonia
no h/o memory loss
no h/o emotional lability
MMSE- 30
cranial nerves- intact
MOTOR SYSTEM
Right. Left
Bulk: inspection NORMAL NORMAL
palpation. NORMAL NORMAL
Measurements U/l 28.5cm. 28.5cm
L/L 37 cm 37 cm
Tone: ul. NORMAL NORMAL
LL. NORMAL NORMAL
Power UL.
Biceps 5/5. 5/5
Triceps 5/5 5/5
Supinator 5/5 5/5
iliopsoas 4+/5. 4+/5
adductor femoris 4+/5. 4+/5
gluteus medius 4+/5. 4-/5
gluteus maximus 4-/5. 4+/5
hamstrings 4+/5. 4+/5
quadriceps femoris 4+/5. 4+/5
tibialis anterior. 4+/5. 4+/5
tibialis posterior. 4-/5. 4-/5
peroneii. 4-/5. 4-/5
gastronemius. 4+/5. 4+/5
extensor -
digitorum longus. 4+/5. 4+/5
flexor digitorum longus 4+/5. 4+/5
Superficial reflexes
Right. Left
Corneal. P P
Conjunctival P. P
Abdominal. + +
Plantar mute extensor
cremasteric. + +
Deep tendon reflexes
Right. Left
Biceps. ++ + ++
Triceps. ++. ++
Supinator. +++ ++
Knee +++ +++
Ankle. ++ ++
SENSORY SYSTEM
SPINOTHALAMIC
crude touch . N. N
pain. N. N
temperature . N. N
post:
fine touch. N. N
vibration. N. N
position sensor. N. N
cortical
2 point discrimination N. N
tactile localisation. N. N
CEREBELLUM
titubation - absent
ataxia - absent
hypotonia. Normal Normal
Based on above findings the following investigations were done::-
INVESTIGATIONS
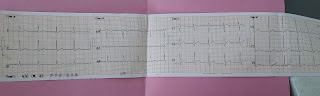
ECG:__
CHEST X-RAY PA VIEW::--
SEROLOGY::--
HIV -- NEGATIVE
HCB antibodies -- NEGATIVE
HbsAg antibodies -- NEGATIVE
CUE:--
Urine- pale yellow colour., Appearence is clear., specific gravity :- 1.010., albumins and sugars are nil. Bile salts and Bile pigments - Nil.,, Pus cells:- 3-4., RBC , CRYSTALS, CASTS-- NIL
RBS::--
CBP :
HB 13.9gm/dl
Platelets 1.5lakhs/cumm
TLC 7,500 cells/cumm
Neutrophils 70%
lymphocytes 25%
smear -normocytic normochromic anemia
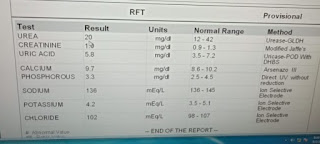
RFT::--
Sr. Urea 39
Sr. Creatinine 3.5
Uric acid 3.0
Na+ 137 meq/l
k+. 3.7meq/l
cl-. 101meq/l
Calcium 9.2
TREATMENT GIVEN :-
1.INJ.OPTINUERON 1ampoule in 100ml NS IV
2. Tab. Pan 40mg OD
DAY.-2 :-
The patient felt subjectively better compared ot yesterday .
-- when asked to remove his shirt ., he felt a little difficulty in his grip.
Treatment given on day 2:-
1.Inj . Optinueron 1amp in 100ml NS iV
2. Tab. Ultracet BD
Advices at Discharge
Follow Up
When to Obtain Urgent Care
Preventive


Comments
Post a Comment